See our section on recent news articles!
See our section on recent news articles!
NEWS:
January 2019 - see the Joint Statement on Stimulating fresh fruit and vegetable consumption for healthier European consumers endorsed by ECL and many other European stakeholders!
Obesity and Cancer: 7 things to know
What are the associations of obesity and cancer?
Obesity and Cancer: 7 things to know
- Obesity is a certain and avoidable cause of many forms of cancer
- Obesity refers to a condition when the body fat proportion is abnormally high
- The percentage of obese adults and children in Europe has increased markedly during the past decades
- Body-mass index (BMI) is a simple and commonly used measurement of obesity
- The link between obesity and cancer is biologically plausible, but the mechanisms are complex, involving multiple interrelated processes that operate at the level of the whole individual (e.g. insulin resistance), in the cancer cell (e.g. the Warburg effect), and in the tumor microenvironment (e.g. inflammation)
- The first recommendation given by the World Cancer Research Fund (WCRF) report is to “be as lean as possible within the normal range of body weight”
- Effects of obesity on cancer development might be specifically curbed through weight-loss through diet, exercise or medication
What are the associations of obesity and cancer?
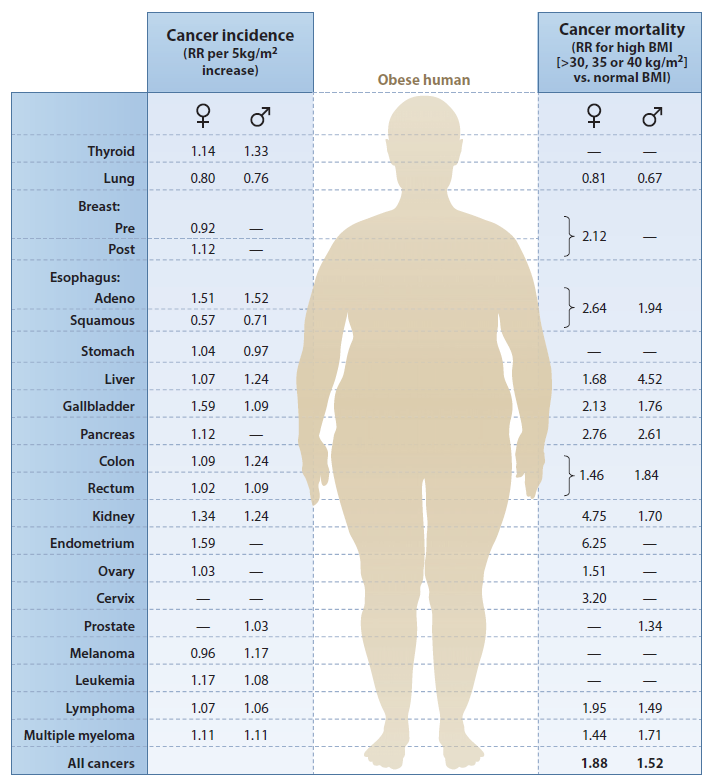
- The relative risks (RRs) of many common cancers were increased in obese individuals, except for the risks of tobacco-associated cancers (lung, esophageal, squamous) (Figure 1)
- Individuals with high body mass indexes (BMIs) (defined as >30, 35, or 40 kg/m2, reflecting the highest category with reliable estimates) were compared to those with BMI 18.5–24.9 kg/m2; the risk of mortality from many common cancers was higher in heavier individuals, except for the risk of lung cancer
- A relative risk of 1 means there is no difference in risk between the two groups
- An RR of small than 1 means the cancer incidence / mortality is less likely to occur in the higher BMI group than the lower BMI group
- An RR of bigger than 1 means the cancer incidence / mortality is more likely to occur in the higher BMI group than the lower BMI group
What is the mechanism underlying the link between obesity and cancer?
- The association of obesity and cancer suggests a complex interplay of factors at multiple levels: the whole individual, the adipose tissue and the tumor cell and its fat-containing microenvironment
- Obesity is associated with expanded and reprogrammed adipose tissue that is metabolically active, leading to localized inflammation and altered cytokine/adipokine secretion
- These local changes contribute to, and interact with, alterations in systemic physiology that reflect the insulin resistance/ metabolic syndrome
- Local adipose tissue and systemic obesity-associated alterations can impact cancer directly by (1) the activation of key signaling pathways or (2) an alteration in cellular metabolism, reflecting an abundance of glucose, free fatty acids (FFAs), and lipids.
- They may also act indirectly on the tumor microenvironment to promote proliferation, angiogenesis, invasion, and epithelial-mesenchymal transition, which may account, in part, for the link between obesity and cancer
- It is unlikely that a single process is primarily responsible the obesity-cancer link
What are some policy strategies for obesity-associated cancer prevention in Europe?
- Taxes on calorically dense, nutritionally sparse foods (e.g. sugar-sweetened beverages)
- Subsidies for healthier foods, especially in economically disadvantaged groups
- Agricultural policies to promote healthy eating through food supply chain
- Urban planning aimed at encouraging walking and other modes of physical activity
References
Campbell, P. T. (2014). Obesity: a certain and avoidable cause of cancer. The Lancet, 384(9945), 727-728.
Calle, E. E., & Kaaks, R. (2004). Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nature Reviews Cancer, 4(8), 579-591.
Calle, E. E., Rodriguez, C., Walker-Thurmond, K., & Thun, M. J. (2003). Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. New England Journal of Medicine, 348(17), 1625-1638.
Goodwin, P. J., & Stambolic, V. (2015). Impact of the Obesity Epidemic on Cancer. Annual review of medicine, 66, 281-296.
Hawkes, c. (March 2013). Linking agricultural policies with obesity and noncommunicable diseases: a new perspective. FAO/WHO Joint Regional Meeting in preparation for the Second International Conference on Nutrition (ICN2).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F., & Zwahlen, M. (2008). Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. The Lancet, 371(9612), 569-578.
World Cancer Research Fund (WCRF) & American Institute for Cancer Research (AICR). (2007). In Food, nutrition, physical activity, and the prevention of cancer: A global perspective (pp 1-537). Washington DC, United States: WCRF and AICR.
The Association of European Cancer Leagues implements activities which receive financial support from the European Commission under an Operating Grant from the European Union's Health Programme (2014-2020). The views expressed on our website and reports do not necessarily reflect the official views of the EU institutions.